Continuing Dementia Following an Episode of Frontal Temporal Lobe Disorder
Overview
What is frontotemporal dementia?
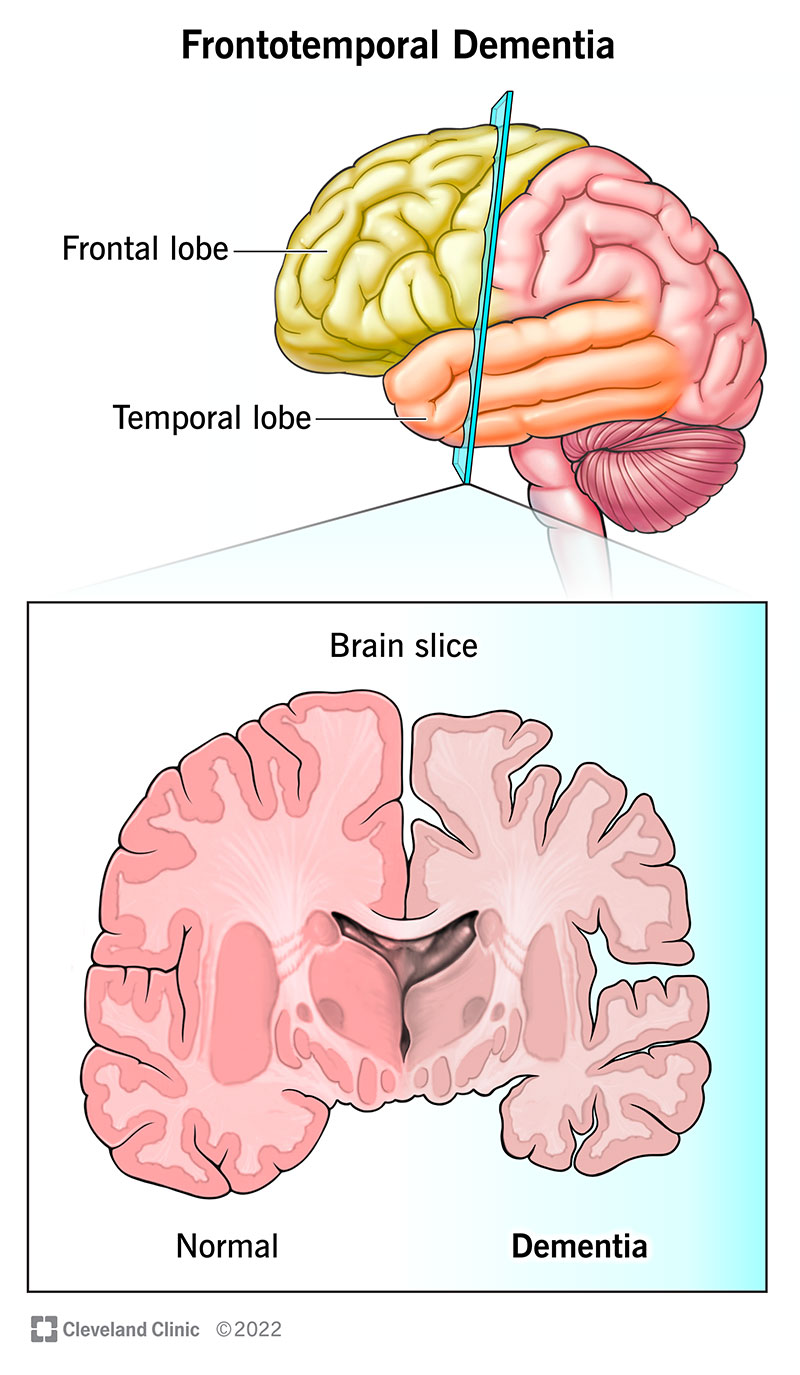
Frontotemporal dementia refers to a group of diseases that involve the deterioration of your brain's frontal and temporal lobes. As those areas deteriorate, you lose the abilities those parts controlled. People with FTD commonly lose control of their behavior or ability to speak and understand spoken language.
People with FTD can fall under one of the three common symptom groups. Two of these are subtypes of primary progressive aphasia (PPA). PPA is a degenerative brain disease. Despite its name, it's very different from the condition/symptom aphasia from conditions like stroke, which affects your ability to speak or understand spoken language. The three common symptom groups are:
- Behavioral-variant FTD (bvFTD).
- Semantic-variant primary progressive aphasia (svPPA).
- Nonfluent/agrammatic primary progressive aphasia (nfvPPA).
Additionally, FTD-related symptoms can occur with these conditions:
- FTD–ALS. When FTD is noted along with amyotrophic lateral sclerosis (ALS).
- Parkinsonian-like FTD syndromes. Parkinson's disease along with progressive supranuclear palsy (PSP) and corticobasal degeneration.
Who does it affect?
Frontotemporal dementia is an age-related condition, but it happens sooner than most age-related conditions that affect your brain. Most people develop FTD conditions between the ages of 50 and 80, and the average age when it starts is 58.
Overall, FTD appears to affect males and females equally. However, the three conditions under FTD don't affect people assigned male at birth and people assigned female at birth equally. Males are more likely to develop bvFTD and svPPA, and females are more likely to develop nfvPP and corticobasal degeneration. FTD is also a condition that can run in families, with about 40% of cases happening in people with a family history of FTD.
How common is this condition?
FTD is an uncommon condition but happens often enough to be fairly well known. Experts estimate that it happens to between 15 and 22 people out of every 100,000. That means between 1.2 million and 1.8 million people have it worldwide.
How does this condition affect my body?
FTD affects your brain's frontal and temporal lobes in the early and middle stages of the disease. As FTD affects those lobes, you lose certain abilities (listed below) because neurons in those areas stop working.
Your frontal lobe, located right behind your forehead, is responsible for the following:
- Movement.
- Planning and decision-making.
- Judgment and reasoning.
- Social skills.
- Spoken language.
- Knowing what's appropriate and inappropriate.
- Self-control over what you do and say.
Your temporal lobes are on the sides of your brain, immediately below and behind your frontal lobe. It handles the following:
- Hearing.
- Understanding spoken language.
- Memory.
- Emotional expression and processing.
Symptoms and Causes
What are the symptoms?
The symptoms of FTD depend on the affected parts of the brain. Even among identical twins, no two brains are the same, so FTD affects everyone differently. Many of the symptoms are similar, but they often happen in different combinations, or they might be more or less severe.
The symptoms of bvFTD fall under six categories:
- Loss of inhibitions.
- Apathy.
- Loss of empathy.
- Compulsive behaviors.
- Changes in diet or mouth-centered behaviors.
- Loss of executive function.
Loss of inhibitions
Inhibition is when your brain tells you not to do something. Losing your inhibitions because of frontal lobe deterioration can look like any of the following:
- Loss of the "filter" for what you say. When this happens, you might say hurtful, rude or offensive things. For some people, this can seem like a major personality shift.
- Lack of respect for others. This often involves getting too close to people (ignoring their personal space) or touching them in unwelcome ways. Inappropriate sexual comments or actions are also common.
- Impulsive actions and behaviors. These are usually risky behaviors, such as reckless gambling or spending. Criminal behaviors like shoplifting are also possible.
Apathy
Healthcare providers commonly mistake apathy for depression because the two have many similarities. Apathy tends to look like the following:
- Loss of motivation.
- Social isolation.
- Decline in self-care and hygiene.
Loss of empathy
People who have a loss of empathy (sometimes known as "emotional blunting") may have trouble reading the emotions of others. That may look like they're behaving in a cold, unfeeling or uncaring way.
Compulsive behaviors
People with FTD often behave in noticeably different ways from people without this condition. Sometimes, behavior changes are small and happen in very limited ways. For others, the changes might be more complicated, involving multiple steps or a strict routine. Some examples include:
- Repetitive motions. People with FTD often repeat small-scale movements, such as clapping their hands, tapping their feet, pacing, etc.
- Complex or ritual-like behaviors. Compulsively watching the same movies, reading the same books or collecting types of items. Hoarding items also falls under this category.
- Speech repetition. A person with FTD may repeat the same sounds, words or phrases.
Changes in diet or mouth-centered behaviors
People with FTD often have a symptom known as "hyperorality," which means they overeat, eat things that aren't food (this is a condition known as pica), or have mouth-centered compulsive behaviors (like smoking or using their mouth to feel things in a way similar to normal exploring behavior in babies).
Loss of executive function without losing other abilities
Executive function is your ability to plan and solve problems, stay organized and motivate yourself to carry out tasks. People with FTD have trouble with executive function, but other abilities like how you process what you see and your memory aren't affected until later stages of the disease.
Primary progressive aphasia
There are three main subtypes of PPA, two of which can happen with FTD:
- Nonfluent variant (nfvPPA). This type involves problems with grammar and forming words. Individual words and simple sentences are understandable, but complicated sentences could cause confusion.
- Semantic variant primary progressive aphasia (svPPA). This type involves problems with choosing and understanding words. People with this often say things that don't make sense or can't understand what other people are saying.
What causes frontotemporal dementia?
FTD happens when neurons, a key type of brain cell, deteriorate. This usually happens when there's a malfunction in how your body creates certain proteins. A key part of how proteins work is their shape. Much like how a key won't turn or open a lock if it's not the right shape, your cells can't use proteins when they're not the right shape. Your cells often can't break those faulty proteins down and get rid of them.
With nowhere to go, those misshapen proteins can tangle and clump together. Over time, these faulty proteins accumulate in and around your neurons, damaging those cells until they don't work at all. Experts have linked misfolded proteins with FTD and its related conditions, such as Pick's disease. Misfolded proteins also play a role in conditions like Alzheimer's disease.
These protein malfunctions happen with certain DNA mutations. DNA is like an instruction manual for your cells, telling them how to do a specific job. Mutations are like typos in the manual. Your cells strictly follow DNA instructions, so even small mutations can cause problems.
Some DNA mutations run in families, which is why about 40% of FTD cases involve a family history of the disease. Mutations can also happen spontaneously, meaning you developed the mutation and didn't get it from your parents.
While they aren't causes, two other factors can increase the risk of developing FTD. One is having a history of head trauma, which more than triples your risk of developing FTD. Thyroid disease is also linked, making FTD 2.5 times more likely to develop.
Is it contagious?
FTD isn't contagious, and you can't pass it from person to person. However, FTD does run in families, so your chance of developing it increases if you have a family member (especially a parent or sibling) who has FTD.
Diagnosis and Tests
How is it diagnosed?
A healthcare provider, usually a neurologist, can diagnose FTD based on your medical history and a physical and neurological examination (where a healthcare provider looks for signs and symptoms of a problem). Some lab tests are also possible, and imaging tests are important because they can show areas of your brain where deterioration is happening.
In addition to neurological examinations, healthcare providers will often have you do a neurocognitive assessment. In this test, you'll do tasks or answer questions. Based on how you do on the test, providers can identify whether or not you have problems in certain areas of your brain, which can help narrow down (or rule out) whether or not you have FTD.
What tests will be done to diagnose this condition?
The most likely tests for FTD include:
- Computerized tomography (CT) scans.
- Magnetic resonance imaging (MRI) scans.
- Positron emission tomography (PET) scan.
- Lumbar puncture (spinal tap).
- Blood tests.
- Electroencephalography (less common).
Management and Treatment
How is it treated, and is there a cure?
FTD is not curable, and there's no way to treat it directly. It's also impossible to slow the progress of the disease. Healthcare providers may recommend treating some of the symptoms, but this can vary from case to case. Your healthcare provider is the best person to tell you what treatments — if any — they recommend.
How do I take care of myself or manage FTD symptoms?
FTD isn't a condition you can diagnose on your own. Because of that, you shouldn't try to manage the symptoms without first talking to a healthcare provider.
Prevention
How can I prevent FTD or reduce my risk of developing it?
FTD happens unpredictably, so there's no way to prevent it. But, it might be possible to reduce your risk of developing it.
The sole way to reduce your risk of developing FTD is to avoid head injuries. Having a past head injury more than triples your risk of developing FTD. A key way to avoid head injuries is to use safety equipment whenever necessary. Helmets and safety restraints (especially seat belts in moving vehicles) can help prevent head injuries or reduce how severe they are if they happen.
Outlook / Prognosis
What can I expect if I have this condition?
FTD is a degenerative brain disease. That means that the effects on your brain get worse over time. Memory loss isn't usually a problem until later in the disease, but other symptoms and effects are likely. Depending on the type of FTD you have, you'll likely lose one of the following:
- Control over your behavior.
- Ability to speak.
- Ability to understand others when they speak.
People with FTD commonly also develop a problem known as anosognosia. This means "lack of insight," and it causes a problem with how your brain processes symptoms or evidence that you have a medical condition. That means you lose the ability to tell that you have a medical condition and to understand what this means for you in the long run.
Because this condition gradually affects your ability to control your actions or communicate, most people who have it eventually can't live independently. Commonly, people with this condition need 24/7 skilled medical care, such as in a skilled nursing facility or long-term care setting.
How long does FTD last?
FTD is a permanent, life-long condition.
What's the outlook for this condition?
FTD gradually affects more and more areas of your brain, disrupting the abilities those areas control. The average life expectancy for a person after diagnosis with FTD is 7.5 years.
While FTD isn't fatal on its own, it often causes other issues that are serious or even life-threatening. One common problem that often happens as FTD gets worse is dysphagia (trouble swallowing). Having dysphagia causes problems with eating, drinking and speaking, and increases the risk of developing pneumonia or respiratory failure.
How can I ensure my wishes are followed when I can't choose myself?
If you have an early diagnosis of frontotemporal dementia of any kind, you may want to talk to your healthcare provider, your family or loved ones, and to anyone you trust to make important decisions for you. These discussions are important because they can help you ensure caregivers can honor your wishes if you can't choose for yourself in the future.
While these conversations often feel unpleasant or difficult, having them sooner rather than later can help avoid confusion about what you want for yourself in the years to come. They also mean your loved ones don't face the painful, difficult situation of having to guess what you wanted.
In addition to those conversations, you should also put your wishes and decisions in writing. That includes preparing documents connected to legal issues and what happens if you can't care for yourself or make decisions for your care or well-being. Many people choose to consult an attorney when preparing these documents. However, many of these are ones you can prepare on your own (you may need a notary or other official to endorse them, depending on the laws in your area).
Living With
How do I take care of myself?
Having FTD means you'll eventually need long-term care because the condition affects your ability to care for yourself. Your healthcare provider can tell you more about what to expect with this. They can also direct you to resources on care options and services that might help you (or your loved one, if you're a caregiver).
Frequently Asked Questions
What can I do if a loved one shows signs of frontotemporal dementia or a similar condition?
People with FTD often lack insight, which means they can't recognize their symptoms or condition. Because they can't see the problem, they often don't believe they need medical care or treatment. That lack of understanding can lead to frustration or fear for the person with the symptoms and their loved ones.
If you notice a loved one showing signs of FTD or a related condition, you can try to help them by doing the following:
- Ask how you can help. People with FTD may show symptoms without realizing that these are symptoms of a serious brain problem. Listening and offering help can help them feel connected and may encourage them to see a healthcare provider.
- Encourage them to see someone who can help. Frontotemporal dementia is a condition that isn't treatable or curable, but some of the symptoms might be treatable. Treatment can sometimes improve the quality of life for a person with this condition or make it easier for loved ones to care for them. Specialized care can offer some relief from some of the disabling symptoms for people with this condition or for loved ones who are caregivers.
- Stay calm and don't take things personally. People with FTD often can't control their behaviors or the things they say. This may cause misunderstandings and is often embarrassing or hurtful. However, it's important to remember that this is a medical problem and not a problem that a person with FTD can control.
- Don't be afraid to ask for assistance. Caring for someone with FTD often gets more difficult, especially as the condition worsens. If you're caring for someone with FTD, don't be afraid to ask for help or resources. There are often support systems and services available. These resources and services include adult day care, respite and home health nursing care.
- Long-term care might be the best option. Caring for a loved one with FTD can be as difficult and require as much effort as a full-time job. Unfortunately, not everyone has the time or ability to care for a loved one with FTD. That means it's important to consider if your loved one needs long-term, skilled care in a specialized facility. Though this isn't an easy choice to make, it's often the best option to make sure your loved one is safe, comfortable, and has qualified people caring for them at all times.
Are there stages of frontotemporal dementia?
While experts have established numbered stages for other degenerative brain conditions such as Alzheimer's disease, there isn't a numbered system for FTD. That's because FTD can happen in different ways and affects every person differently.
What is the life expectancy of FTD?
The average life expectancy after a diagnosis of FTD is 7.5 years. But the condition can progress faster or slower. Your healthcare provider (or the provider for your loved one) is the best person to tell you more about the progress of the disease and the likely timeline. They can also update you throughout the course of the disease if it progresses faster or slower than expected.
Is FTD worse than Alzheimer's disease?
FTD and Alzheimer's disease are both conditions that can severely affect and disrupt a person's life. Generally, FTD affects people at a younger age than Alzheimer's disease. But there's no way to define whether one condition is better or worse than the other because these conditions affect everyone differently.
What are the early signs of frontal lobe dementia?
When frontotemporal dementia affects the frontal lobe first, this causes the behavioral variant of this condition. The earliest signs and symptoms of this condition include:
The symptoms of bvFTD fall under six categories:
- Loss of inhibitions. This means a person has trouble controlling themselves. That can lead to them making inappropriate comments or behaving in socially unacceptable ways.
- Apathy. This usually causes a lack of interest or motivation. This is often similar to (or mistaken for) depression.
- Loss of empathy. This means a person has trouble reading other people's emotions or acts as if they don't care about the feelings of others.
- Compulsive behaviors. This usually means repetitive movements or behaviors that they can't control.
- Changes in diet or mouth-centered behaviors. This usually causes people with FTD to overeat or eat things that aren't food. They may also put things in their mouth, similar to how babies do as they explore objects around them.
- Loss of executive function. This causes a person to have trouble planning, carrying out tasks or motivating themselves to do certain things.
A note from Cleveland Clinic
Frontotemporal dementia is a long-term condition that eventually impacts a person's ability to control their behavior or to speak and understand others speaking to them. Over time, it eventually disrupts a person's ability to think, care for themselves and live independently. Because of how severe the effects are, people who have this condition may want to consider putting their wishes or instructions for their care in writing as soon as possible.
Unfortunately, this condition isn't curable, and there's no standard treatment. It's sometimes possible to treat the symptoms, but this varies from person to person. Eventually, most people with this condition need 24/7 care from skilled healthcare professionals.
houstonthounfor1944.blogspot.com
Source: https://my.clevelandclinic.org/health/diseases/21075-frontotemporal-dementia
Post a Comment for "Continuing Dementia Following an Episode of Frontal Temporal Lobe Disorder"